TMJ vs. Sleep Apnea: Understanding the Connection, Symptoms, and Dental Treatment Options
Temporomandibular joint disorders (TMJ or TMD) and sleep apnea are distinct conditions that often intersect through shared anatomy and functional consequences, and understanding their connection can speed diagnosis and improve outcomes. This article explains how jaw position, airway mechanics, and sleep-related muscle activity link TMJ, obstructive sleep apnea (OSA), and bruxism, and it offers clear guidance on symptoms, dental diagnostic workflows, and dental treatment options. Readers will learn to recognize overlapping signs such as morning headaches, grinding, and jaw pain, and to follow a practical diagnostic pathway that dentists use to evaluate both bite and airway. The goal is to map evidence-based interventions — from oral appliance therapy to orthodontics and restorative work — to patient journeys so people can make informed decisions and seek coordinated care. Below you will find sections that explain the anatomical connection, compare symptoms with a clinical table, describe the dental diagnostic workflow, review dental treatments with a treatment EAV table, outline self-care strategies, and explain why Village Dental Group is positioned to provide integrated, gentle care for this complex intersection of dental and sleep health.
What Is the Connection Between TMJ Disorders and Sleep Apnea?
TMJ disorders and sleep apnea are linked primarily by jaw position and neuromuscular activity that influence airway patency and joint loading. Anatomically, the mandible’s position determines tongue and soft-tissue relationships with the pharyngeal airway, and posterior displacement of the mandible can reduce airway space during sleep, promoting collapse and obstructive events. Functionally, sleep-disordered breathing produces arousals and oxygen fluctuations that can trigger sleep bruxism, increasing masticatory muscle activity and mechanical stress on the temporomandibular joint. Recognizing this bidirectional relationship clarifies why treating one condition often affects the other and why a coordinated diagnostic approach benefits patients with overlapping symptoms. The mechanisms below summarize the main pathways linking TMJ and sleep apnea and lead into specific anatomical and physiological details.
- Jaw position can narrow the airway and increase collapse risk during sleep.
- Sleep apnea can trigger bruxism and repetitive jaw loading, worsening TMJ symptoms.
- Shared risk factors such as obesity, craniofacial structure, and airway anatomy make co-occurrence more likely.
This mechanistic overview sets up the next sections that explore mandibular mechanics and the role of bruxism in more detail.
How Does Jaw Misalignment Affect Airway Obstruction?
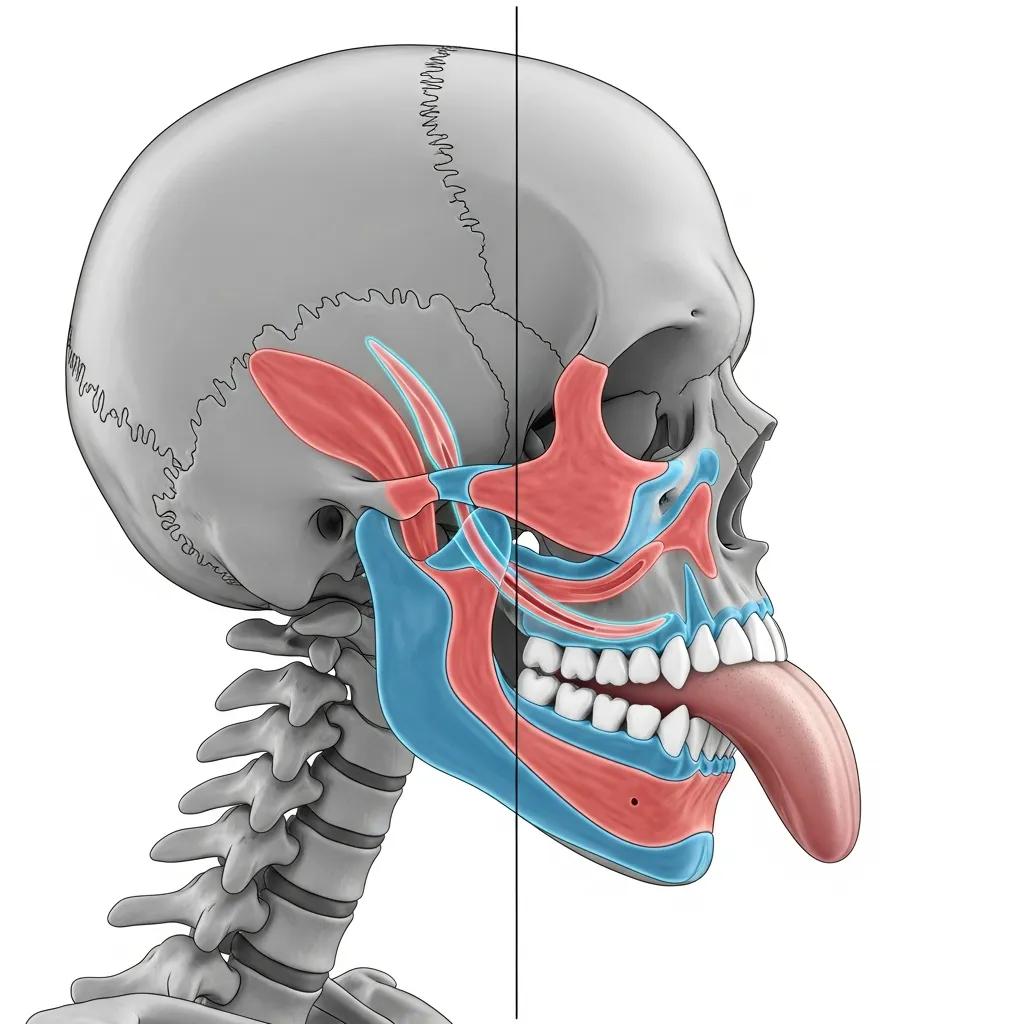
Jaw misalignment alters the spatial relationship of the mandible, tongue base, and soft palate, which directly affects airway calibre during sleep. When the mandible sits posteriorly (retrognathia) or when occlusion forces the jaw into a retruded position, the tongue and soft palate move closer to the posterior pharyngeal wall, increasing the likelihood of airway collapse on inspiration. Clinically, advancing the mandible with a mandibular advancement device (MAD) enlarges the posterior airway space and reduces obstruction events, which explains why dentally delivered appliances can be effective for many patients with mild-to-moderate OSA. Understanding this mechanical link helps clinicians decide when jaw-focused dental strategies — such as orthodontics or appliance therapy — are appropriate as part of airway management. The mechanical concepts here transition to how muscle activity during sleep interacts with these structural factors.
Why Is Bruxism a Shared Symptom and Cause of TMJ and Sleep Apnea?
Sleep bruxism frequently accompanies obstructive events and brief arousals; it is both a symptom and a response to disturbed sleep architecture. Physiologically, respiratory effort and transient hypoxia can trigger micro-arousals that increase sympathetic activity and clench or grind the teeth, producing high masticatory loads on the TMJ and associated muscles. Repetitive grinding increases joint stress, inflammatory responses, and muscular pain, which can perpetuate TMJ symptoms even when airway events are reduced. Recent studies indicate that treating OSA — for instance, by reducing obstructive events — often lowers bruxism frequency, which in turn can alleviate TMJ strain and pain. Recognizing bruxism as a mediator between sleep-disordered breathing and TMD frames the value of integrated assessment and therapy strategies that address both airway and occlusion.
What Are the Common Symptoms of TMJ and Sleep Apnea to Recognize?
Both TMJ disorders and sleep apnea have distinct hallmark symptoms and a set of overlapping signs that can cause diagnostic confusion if viewed in isolation. TMJ-specific complaints include jaw pain, popping or clicking, limited opening, and pain with chewing, while sleep apnea more commonly presents with loud snoring, witnessed apneas, and daytime sleepiness. Overlapping symptoms — such as morning headaches, bruxism, ear or facial pain, and disrupted sleep — should prompt clinicians to screen for both conditions during assessment. Below is an EAV-style comparison table to help readers and clinicians rapidly distinguish typical presentations and note overlap cues that guide the diagnostic pathway.
This comparison highlights distinguishing features and transitional clues clinicians use to decide on further testing and referrals, which is described next.
Which Symptoms Indicate TMJ Disorders?
TMJ disorders most commonly manifest as localized jaw pain, audible joint sounds (clicking or crepitus), episodes of jaw locking or limited range of motion, and pain during mastication. Patients may also report referred pain to the ear, temple, or neck, and show palpation tenderness of the masseter and temporalis muscles on clinical exam. Severity ranges from intermittent discomfort to persistent functional limitation that interferes with eating and speaking, and progressive symptoms should prompt thorough occlusal and joint evaluation. Differentiating TMJ pain from odontogenic or sinus pain relies on a structured exam and targeted imaging when indicated, which transitions to screening for concurrent sleep-related contributors.
What Sleep Apnea Symptoms Overlap with TMJ?
Symptoms that commonly overlap include morning headaches, bruxism, nonrestorative sleep, and daytime fatigue, which can be mistakenly attributed solely to dental causes or to primary sleep disorders. Snoring and witnessed apneas point more strongly to obstructive sleep apnea, while joint locking and mechanical jaw limitations favor TMJ, but many patients exhibit both clusters concurrently. Clinicians watch for red flags — loud snoring, choking episodes, and excessive daytime sleepiness — that necessitate sleep-focused testing alongside a TMJ workup. Appreciating this overlap supports an integrated diagnostic plan that reduces the risk of treating one problem while missing the other.
How Are TMJ Disorders and Sleep Apnea Diagnosed by Dental Professionals?
Dental professionals use a structured workflow that begins with screening questions and a clinical TMJ exam, proceeds to targeted imaging and airway evaluation, and culminates in sleep testing or an appliance trial when indicated. The dental diagnostic pathway emphasizes a stepwise approach: screen, examine, image, test, and treat or refer, which clarifies decision points for appliance therapy, orthodontic intervention, or medical referral. Below is a diagnostic EAV table that outlines typical steps, what each step reveals, and the next actions or referrals it suggests. After the table, a concise numbered workflow summarizes clinician actions that patients can expect during evaluation.
This table clarifies how each diagnostic phase informs treatment planning and referral needs and sets up the practical step-by-step workflow described next.
- Conduct screening questions and validated questionnaires to assess risk for sleep apnea and TMJ symptoms.
- Perform a focused TMJ exam including range-of-motion, palpation of masticatory muscles, and occlusal evaluation.
- Order imaging when structural or airway concerns are suspected to guide orthodontic or restorative planning.
- Arrange home sleep testing or referral to a sleep physician if screening suggests obstructive events; consider an appliance trial under dental supervision.
These steps form the decision pathway dentists use to coordinate care, and briefly exemplify how a local practice may support comprehensive diagnostics. Village Dental Group, with in-house specialists and advanced technology, follows a similar workflow to provide coordinated screening, imaging, and appliance fitting when appropriate, while collaborating with sleep medicine providers as needed. This capability supports a seamless referral and follow-up path for patients transitioning from screening to definitive treatment.
What Is the Diagnostic Process for TMJ Disorders?
Diagnosing TMJ disorders begins with a structured clinical exam that documents pain locations, joint sounds, range of motion, and functional limitations such as difficulty chewing or jaw locking. Palpation of the masseter, temporalis, and other masticatory muscles maps pain referral patterns, while occlusal assessment evaluates bite relationships that may contribute to joint loading. When indicated, imaging such as panoramic films or cone-beam CT clarifies bony anatomy and occlusal vertical dimension to guide restorative or orthodontic interventions. If conservative measures fail or structural anomalies are present, referral to in-house specialists or external colleagues is considered for advanced management, linking the diagnostic process to subsequent treatment planning.
How Do Dentists Diagnose Sleep Apnea?
Dentists screen for sleep apnea using questionnaires, clinical airway assessments, and examination of craniofacial risk factors such as retrognathia or reduced posterior airway space. Positive screens lead to coordination with sleep physicians for home sleep apnea testing or polysomnography, which quantifies obstructive events and informs treatment choices. Dentists may then provide an appliance trial — custom-fitted and titrated — under dental sleep medicine protocols while maintaining communication with the sleep physician regarding effectiveness and side effects. This collaborative model ensures dental interventions for airway are evidence-informed and medically coordinated.
What Dental Treatment Options Address Both TMJ and Sleep Apnea?

Dental care offers several interventions that can address TMJ symptoms while also reducing airway obstruction risk, including oral appliance therapy, orthodontic corrections, and restorative approaches that re-establish occlusion. Oral appliance therapy, particularly mandibular advancement devices (MADs), repositions the mandible forward to enlarge the posterior airway space and often reduces bruxism-related loading by changing occlusal contacts. Orthodontic options can alter jaw relationships and improve occlusion, indirectly enhancing airway patency in select patients; restorative dentistry and implants restore vertical dimension and bite stability, reducing maladaptive joint mechanics. Below is a treatment EAV table summarizing common dental modalities, their mechanism, and when they are typically indicated.
- Oral appliance therapy can reduce obstructive events and mitigate bruxism by repositioning the jaw.
- Orthodontic treatment may be appropriate to change skeletal relationships or correct malocclusion that contributes to airway compromise.
- Restorative dentistry and implants rebuild occlusion when tooth loss has led to bite collapse and TMJ overload.
Village Dental Group offers coordinated services that match these treatment pathways, including custom oral appliance therapy, orthodontic care, restorative dentistry, and implant solutions, delivered with an emphasis on holistic planning and patient comfort. Patients at the practice can expect an evaluation pathway that includes screening, imaging, appliance fitting or orthodontic planning, and follow-up to balance airway benefit with TMJ comfort.
How Does Oral Appliance Therapy Treat TMJ and Sleep Apnea?
Oral appliance therapy uses custom mandibular advancement devices (MADs) to reposition the mandible forward, mechanically enlarging the posterior airway space and reducing obstruction during sleep. This forward positioning also changes dental contacts and masticatory muscle activity, which can reduce bruxism episodes and lower peak loads on the TMJ, although careful titration is required to avoid aggravating joint discomfort. Devices are custom-made from dental impressions and adjusted over several visits to find the optimal balance between airway improvement and joint comfort; follow-up monitoring ensures side effects such as tooth movement or soreness are managed.
For patients with mild to moderate OSA or those intolerant of CPAP, MADs represent an evidence-based dental option that simultaneously addresses sleep-disordered breathing and bruxism-related TMJ strain.
What Orthodontic Solutions Improve Jaw Alignment and Airway Function?
Orthodontic approaches include functional appliances for growing patients, conventional braces, and clear aligner therapy to correct malocclusion and improve jaw relationships that affect airway dynamics. In growing individuals, functional appliances can encourage mandibular advancement and potentially expand airway dimensions, while adult strategies may combine orthodontics with surgical options when structural correction is required. Orthodontic treatment can also optimize occlusion and distribute occlusal forces more evenly, reducing chronic TMJ loading; planning often involves interdisciplinary consultation to align airway goals with dental stability. Selecting candidates requires careful assessment of skeletal pattern, airway anatomy, and TMJ status to ensure interventions support both breathing and joint health.
How Can Restorative Dentistry and Dental Implants Help TMJ and Sleep Apnea?
Restorative dentistry — including crowns, full-mouth reconstruction, and dental implants — re-establishes proper occlusal relationships and vertical dimension, which can reduce maladaptive joint mechanics that drive TMJ pain.
When missing teeth cause bite collapse or uneven force distribution, implants and prosthetic restorations can restore stable contacts and improve masticatory efficiency, indirectly reducing TMJ strain.
While restorative treatments primarily target occlusion and TMJ function, they become part of an integrated airway plan when combined with appliance therapy or orthodontics that address mandibular position.
In practice, coordinated restorative and airway-focused plans improve function, comfort, and long-term outcomes for patients with overlapping TMJ and sleep-disordered breathing.
How Can Patients Manage TMJ and Sleep Apnea Symptoms for Better Quality of Life?
Patients can adopt several practical self-care measures and lifestyle changes that complement professional treatments and improve sleep quality and jaw comfort.
- Weight management, avoiding alcohol and sedatives before bedtime, and optimized sleep position (favoring side-sleeping) reduce obstructive events and nighttime arousals that drive bruxism.
- For TMJ symptom relief, jaw exercises, controlled soft-diet periods, heat or cold therapy, and stress-reduction techniques lower muscle tension and pain while awaiting definitive dental care.
- Regular follow-up, appliance maintenance, and multidisciplinary coordination yield sustained improvements and reduce recurrence, which leads to a maintenance timeline discussed in the next subsection.
What Lifestyle Modifications Support TMJ and Sleep Apnea Treatment?
Lifestyle adjustments that reduce airway collapsibility and masticatory tension include weight reduction, avoidance of evening alcohol or sedatives, and choosing side-sleeping positions that promote airway patency.
Stress management practices such as biofeedback, mindfulness, and targeted jaw relaxation exercises help decrease parafunctional grinding and clenching that exacerbate TMJ pain.
Maintaining consistent sleep schedules and optimizing bedroom environment improve sleep continuity, lowering arousal frequency that can trigger bruxism.
These changes are practical, noninvasive complements to dental interventions and often form the first-line recommendations while diagnostic and appliance processes proceed.
How Can Pain and Sleep Quality Be Improved Long-Term?
Long-term improvement hinges on adherence to prescribed therapies, routine appliance maintenance, periodic reassessment, and coordinated multidisciplinary care for persistent or complex cases.
For oral appliances, regular dental checkups ensure fit and function while monitoring dental alignment and TMJ status; for orthodontic or restorative care, staged follow-up secures occlusal stability and airway outcomes.
When progress plateaus, coordinated referrals to sleep medicine, physical therapy, or pain specialists refine management and address residual sleep or pain issues.
A maintenance timeline with scheduled reviews every few months initially, then annually, helps detect changes early and sustain quality-of-life gains over time.
Why Choose Village Dental Group for TMJ and Sleep Apnea Care in South Orange, NJ?
Village Dental Group provides a family-oriented, holistic approach that integrates in-house specialists and advanced dental technology to evaluate and manage the complex interplay of TMJ disorders and sleep-disordered breathing.
The practice emphasizes gentle, pain-free techniques that benefit patients with dental anxiety and offers coordinated care pathways involving orthodontic and periodontal expertise alongside general dentistry.
With a focus on whole-patient health, Village Dental Group combines screening, imaging, custom appliance fabrication, and restorative planning to address both occlusion and airway concerns in a unified plan.
For patients seeking local, compassionate care for overlapping TMJ and sleep issues, this integrated model supports streamlined diagnosis, appliance titration, and long-term follow-up.
What Makes Our Holistic and Gentle Approach Unique?
The practice philosophy centers on treating oral health within the broader context of overall wellbeing, recognizing that jaw function, airway health, and sleep quality are interdependent components of patient health.
Gentle care strategies reduce fear and improve treatment adherence, while collaborative planning among clinicians ensures that appliance therapy, orthodontics, and restorative work align with airway goals.
By coordinating diagnostics and follow-up, the practice reduces fragmentation of care, which leads to more predictable outcomes and less patient burden.
This holistic orientation directly supports patients who need both TMJ symptom relief and airway-focused interventions.
Who Are the Specialists Treating TMJ and Sleep Apnea at Village Dental Group?
Village Dental Group’s team includes general dentists who manage screening and appliance fabrication, as well as in-house specialists such as an orthodontist and a periodontist who contribute to complex treatment planning and restorative solutions.
Clinicians within the practice — including Dr. Christian, Dr. Simmonds, and Dr. Copeland — collaborate to create integrated care pathways that balance airway improvement with occlusal stability and patient comfort.
This multidisciplinary team approach allows patients to receive coordinated diagnostics, appliance titration, orthodontic adjustments, and restorative planning within one supportive environment, reducing care fragmentation and improving long-term outcomes.